About the Project
The Problem of Readmissions
Readmissions cause both emotional and financial stress for patients and caregivers. Many of these readmissions can be prevented if patients better understood how to care for themselves following their hospital discharge.
Readmissions & Discharge Planning
UPMC Enterprises charged our team with coming up with a solution to help reduce readmissions by exploring the discharge planning process.
We were asked to create a tool that addressed factors outside the hospital that are critical to patient outcomes, like a patient’s support system, transportation, access to follow-up care and more. Our task was to support clearer communication and planning around these “soft factors” during care transitions, ultimately reducing a patient’s risk for readmission.
Patient‑Provider Collaboration
- Providers can better understand patients’ lives outside the hospital.
- Patients can more fully clarify, understand, and even shape and co-create their plans.
- Chronic disease patients’ adherence to care instructions will improve, due to a sense of ownership and empowerment, leading to better health outcomes and reduced readmission rates.
Our Vision
Discovery Methods
Understanding The Problem Space
We conducted research to gain an end-to-end view of discharge planning by looking at a patient’s journey from hospital stay, to discharge, to the home.
Researching The Domain
Literature Review
Healthcare Landscape
Our Competitors
Exploring The Patient’s Journey

Interviews
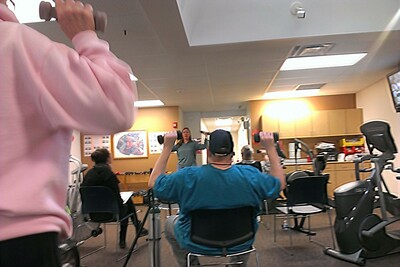
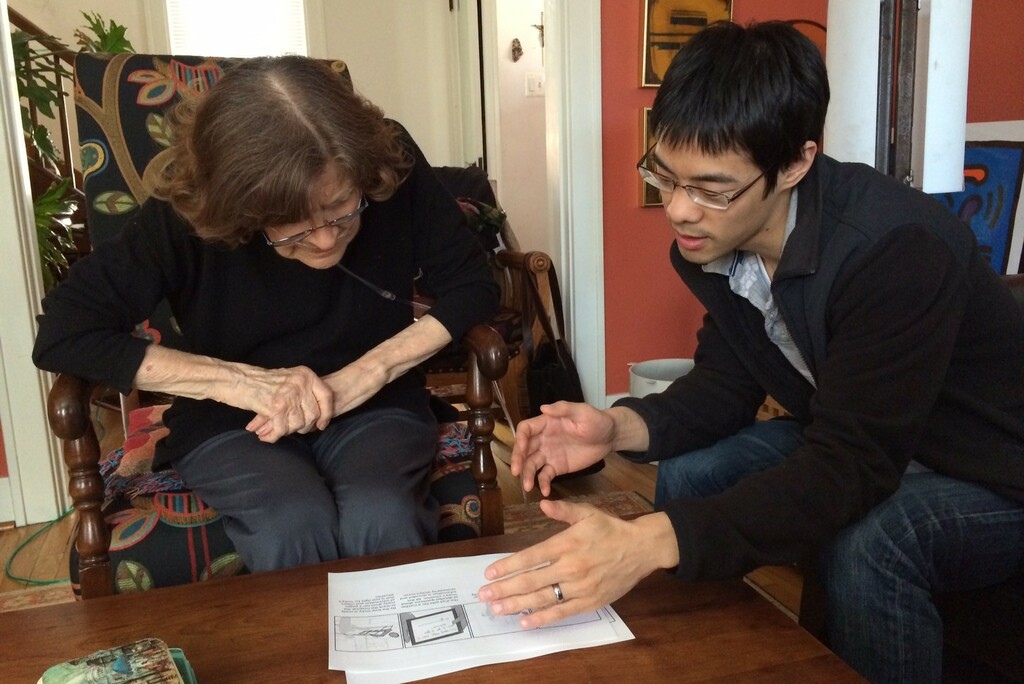
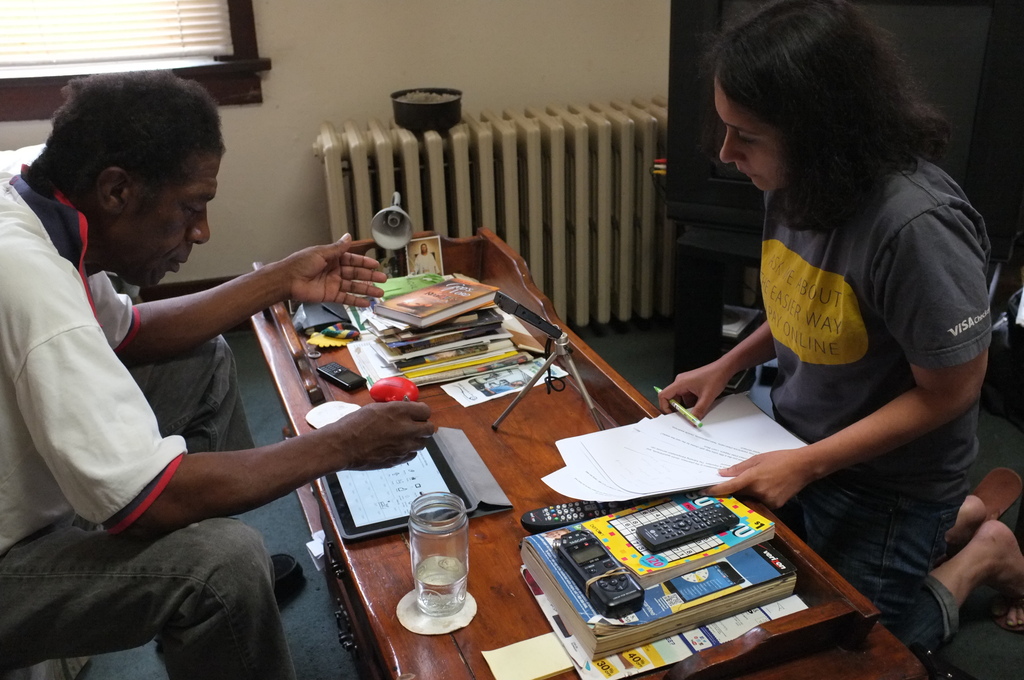
To gain in depth understanding of a patient’s experience during the discharge process and after, we interviewed over 15 patients who were recently discharged from the hospital. We also visited them in their homes to see where they kept their discharge packets and how they managed their complex medication regimen.
Diary Studies
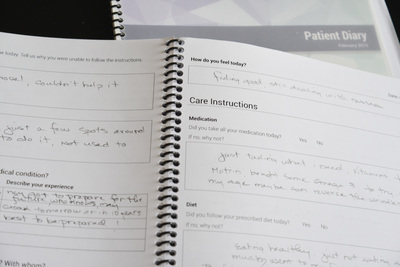
We gave diaries to patients so they could record their thoughts and feelings for 10 days after discharge from the hospital. They also recorded if they were able to follow their care instructions each day, as well as personal obstacles and challenges that made following instructions difficult.
Synthesis
Generating Insights from Our Research

Affinity Diagram
Our interviews and shadowing sessions generated over 1,400 notes which we grouped into meaningful clusters using an affinity diagram. We used this process to draw high-level insights that provided the basis for generating design ideas.
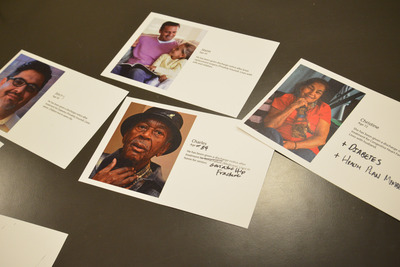
Patient Personas
Through our primary research, we discovered the common behaviors, thoughts, and feelings that influence non-compliance, synthesizing these findings to create patient personas. We also used findings from our literature review to decide on the medical conditions and age group for the personas we developed.
Ideation
Establishing a Vision For The Product

Setting the direction
To understand what design ideas would be most feasible and have the highest impact, we created a short-list of 40 ideas of possible solutions based on 10 of our top findings. We then asked our client to map these ideas to an impact vs. feasibility matrix while explaining their rationale.
Design
Creating a Collaboration Tool
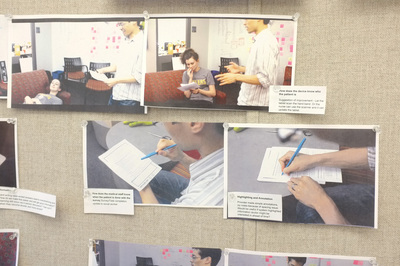
Role Playing
We used generative role-play to brainstorm what tablet interactions might be effective and engaging in the context of a hospital space.
Next Steps
Final Deliverables
- a 3-minute concept video
- a high-fidelity, interactive prototype
- a web-based, functional prototype
- a 40-page research report
- a 40-page design report
- 2 × 40-minute presentations
Piloting at the Hospital
Within our scope and timeframe, we weren’t able to pilot our solution at the hospital. Before implementing our solution, we strongly recommend that UPMC conduct a pilot within the app’s intended environment of use. The pilot should include a sample of patients using OnTrack, and a control group. The effectiveness of OnTrack should be evaluated along the following metrics:
Communication
Does OnTrack reduce miscommunication, helping patients, caregivers, and hospital staff coordinate better?
Workflow
Will OnTrack account for all of the staff’s logistical challenges, or should some revisions be made?
Adoption
Do hospital staff continue to use the inpatient component of OnTrack through the entire length of the pilot? Do patients continue to use the outpatient component of OnTrack for the entire 30- days after discharge?
Adherence
Are patients using the inpatient and outpatient components of OnTrack more likely to adhere to their care instructions than the control group?
Reduced Readmissions
Are patients using OnTrack less likely to be readmitted within 30 days than the control group?
“This application is engaging because it shows interest in me as an individual. These are things about me the hospital should know, and they don’t ask those questions now.” —Mary, Heart Failure Patient
“This is fun! It’s like playing solitaire or bingo!” —Dora, Diabetes Patient
“I think this would be awesome. Especially for someone who is new to medicine, just had a heart attack or something. It would help caregivers, nursing home staff, or a patient who lives alone to have the most important instructions sectioned out and easy to read like this.” —Caregiver

Team Quetzal


Anna Malone
Team Lead
Anna has a background in English, Philosophy and UX Design. Within the field of user-centered design, she aspires to empower people and improve their daily lives.

Diya Deb
UX Lead
Diya has a background in Industrial Design and UX Design. She views user-centered service design systems as a means of introducing positive social change.
Jay Liu
Tech Lead
Jay does UX design, prototyping, and web development. He endeavors to serve and empower people through the effective design of technology.

Mike Szegedy
Design Lead
Mike has over 10 years of industry experience in interaction design and UX research. He enjoys difficult problems and exploring new design spaces.

Tina Jose
Research Lead
With a background in Design and Psychology, Tina has worked in the digital space for over 10 years. She enjoys finding elegant solutions for complex problems, and sees herself as an advocate for the user.